Listen to the podcast HERE.
WHO AM I? MEET YOUR PELVIC HEALTH PHYSIOTHERAPIST
My name is Gerda Hayden and I am a pelvic health physiotherapist, practicing out of the World of My Baby or WOMB in Burlington, Ontario. I am trained neuro-musculo-skeletal or ‘normal’ physiotherapist but have completed specialised training as a pelvic health physiotherapist which allows me to further assess women via their vagina and/or rectum if that is indicated.
I completed my studies in South Africa and worked in various multi-disciplinary practices, the largest one of which focused on athletes. It was here that I became most aware that we were viewing women, often and inadvertently, as small men. Menstrual cycles and vaginal and bowel or bladder complaints were at best minimised or completely disregarded, and I realised that there was a real need for more pelvic floor specialists to address these concerns.
I did my pelvic health post graduate qualifications while being pregnant with my first son and started a women’s health practice when he was 6 months old.
We then immigrated to the UK, where I had my 2nd son and arrived in Canada in early 2017 where I met my mentor Sinead DuFour and started my journey at the WOMB. It is a perinatal care facility that aims to support women in a very holistic manner.
I have an interest in the perimenopausal space so I really do see a wide range of women. From young competitive athletes to women planning their fertility journey to pregnant and post partum women as well as post menopausal ladies.
WHAT IS PELVIC HEALTH PHYSIOTHERAPY?
Pelvic health physiotherapy looks at the role the pelvis and its contents and tissue are playing in pelvic complaints and overall well-being.
The pelvic floor is made up of muscles, connective tissues, nerves, ligaments and supports the pelvic organs while also facilitating good voiding of the bladder. It allows good sexual functioning and is part of the postural control mechanism.
The muscles run from the coccyx or tailbone all the way to the pubic bone and into the sides of the pelvis.
It is also implicated in good gut health, which we are now understanding is crucial to our immune response and hormone regulation due to its role in voiding of bowel movements.
As a physiotherapist I am really intrigued by the muscular aspect. Broadly speaking the pelvic floor can be underactive, essentially under-supportive, and present with complaints such as prolapse or stress urinary incontinence. On the other side we can classify the pelvic floor as overactive. Presenting complaints are then more along the lines of painful intercourse ( a sense of hitting a wall) , constipation or urinary urgency and frequency.
And then we can also encounter some asymmetries, or co-ordination issues as well as injuries to the pelvic floor.
WHAT CONDITIONS CAN PELVIC HEALTH PHYSIOTHERAPY ADDRESS?
I’m going to unpack all these complaints a bit more, but really want to reiterate that as much as I am focusing on pelvic complaints, I am very mindful and aware of the fact that I am working with a woman whose entire health matters. Her perception of her concern, her overarching well-being, her sleep quality, her stress resilience and nutritional status: ALL of it matters and that conversation takes up just as much time as unpacking the pelvic details.
So let’s unpack those complaints a bit more.
Urinary incontinence
Urinary incontinence is the unintentional loss of urine. Stress incontinence happens when physical movement or activity — such as coughing, laughing, sneezing, running or heavy lifting — puts pressure (stress) on your bladder, causing you to leak urine. Stress incontinence is not related to psychological stress. Stress incontinence is much more common in women than in men.
Stress incontinence occurs when the muscles and other tissues that support the urethra (pelvic floor muscles) and the muscles that control the release of urine (urinary sphincter) weaken.
The bladder expands as it fills with urine. Normally, valve-like muscles in the urethra — the short tube that carries urine out of your body — stay closed as the bladder expands, preventing urine leakage until you reach a bathroom. But when those muscles weaken, anything that exerts force on the abdominal and pelvic muscles — sneezing, bending over, lifting or laughing hard, for instance — can put pressure on your bladder and cause urine leakage.
Your pelvic floor muscles and urinary sphincter may lose strength because of:
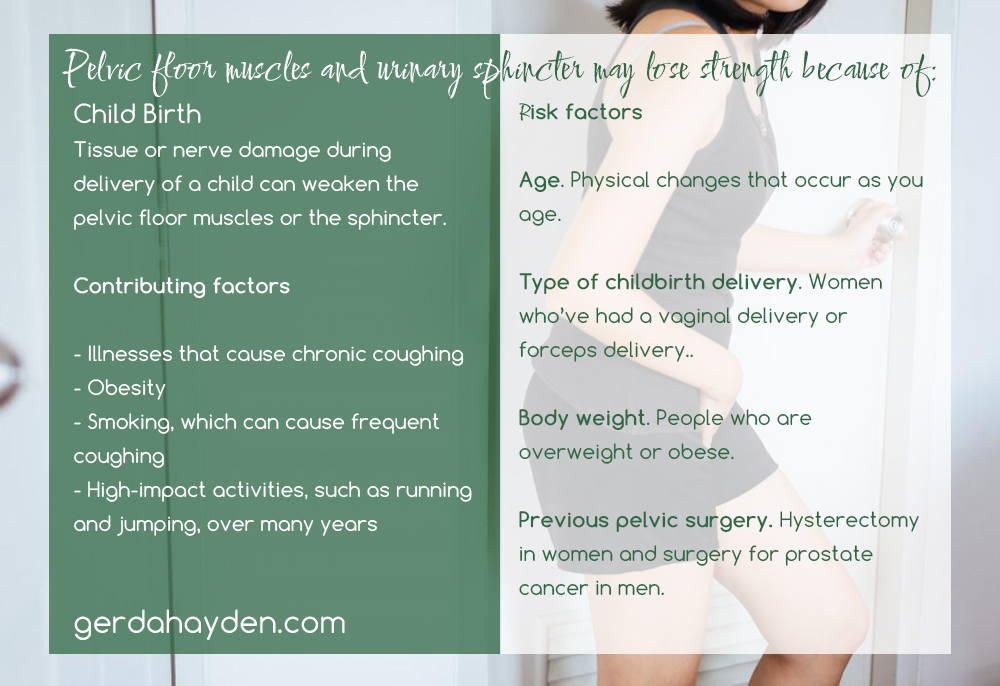
Childbirth. In women, tissue or nerve damage during delivery of a child can weaken the pelvic floor muscles or the sphincter. Stress incontinence from this damage may begin soon after delivery or occur years later.
Contributing factors
Other factors that may worsen stress incontinence include:
- Illnesses that cause chronic coughing
- Obesity
- Smoking, which can cause frequent coughing
- High-impact activities, such as running and jumping, over many years
Risk factors
Factors that increase the risk of developing stress incontinence include:
- Age. Physical changes that occur as you age, such as the weakening of muscles, may make you more likely to develop stress incontinence. However, occasional stress incontinence can occur at any age.
- Type of childbirth delivery. Women who’ve had a vaginal delivery are more likely to develop urinary incontinence than women who’ve delivered via a cesarean section. Women who’ve had a forceps delivery to more rapidly deliver a healthy baby may also have a greater risk of stress incontinence. Women who’ve had a vacuum-assisted delivery don’t appear to have a higher risk for stress incontinence.
- Body weight. People who are overweight or obese have a higher risk of stress incontinence. Excess weight increases pressure on the abdominal and pelvic organs.
- Previous pelvic surgery. Hysterectomy in women and surgery for prostate cancer in men can weaken the muscles that support the bladder and urethra, increasing the risk of stress incontinence.
Stress incontinence is different from urgency incontinence and overactive bladder (OAB). If you have urgency incontinence or OAB, your bladder muscle contracts, causing a sudden urge to urinate before you can get to the bathroom. ( I will address this later in the talk)
A lot of women will present with mixed urinary incontinence which is a combination of SUI and UI.
Prolapse
Another symptom of decreased pelvic support is prolapse. It is often abbreviated to POP for ‘pelvic organ prolapse’ and is the term given to the medical condition in which pelvic organs descend from their normal positions within the pelvic cavity.
It is a common problem reported in as many as 1 in 2 women.
Generally, three main types occur:
- A cystocele, where the bladder (or urethra) descends into the vagina,
- A rectocele, where the rectum descends into the vagina and
- A uterine prolapse, where the uterus (cervix) descends into the vagina.
POP is most often related to repeated strain on the pelvic structures and occurs typically when the pelvic floor muscles are not providing optimal support. So, causes of both strain and pelvic floor damage are triggers of POP. Examples include prolonged 2nd stage in labour, vaginal birth with surgical assistance from forceps or episiotomy, cumulative trauma such as breath- holding, repeated heavy lifting with a poor technique, straining when having a bowel movement and/or persistent coughing are all common culprits.
The most common complaint is of a sense of heaviness, especially towards the end of the day. Other complaints include the sense that something is protruding from the vagina or the feeling of ‘sitting on a ball’. Incomplete emptying or difficulty initiating urination are also often mentioned.
Symptoms vary according to the organ involved. Pain can be a part of the picture but oftentimes the pain is related to other aspects of pelvic dysfunction .
Degree of perceived bother is one of the key aspects I look at. How much does the prolapse impact your activities of daily living and your quality of life. I make this point because there is a lot of debate around whether we should even quantify ‘minor’ prolapses since a degree of tissue laxity is evident in most postpartum and perimenopausal women.
Conservative care strategies are considered the first line management for POP. Research shows that supervised pelvic floor muscle training, guidance related to general movement and diet and the use of adjunct devices called pessaries are very effective.
I also consider hormonal changes in my practice. We know that low estrogen levels contribute to tissue laxity, shrinking and drying of tissue and this can exacerbate symptoms.
This is where working with a hormone literate GP can be really beneficial. The GP can prescribe estrogen supplementation to optimise tissue function. Local estrogen comes in the form of a vaginal tablet, creams or gel or a ring pessary.
In addition to pelvic floor muscles training, lifestyle counselling is a powerful way to manage POP symptoms. Again these will be tailored to meet your needs but generally revolve around these four principles:
Pacing Posturing Planning Practising

If standing aggravates symptoms, try and do the bulk of standing activities earlier in the day and pace yourself while doing them. Intersperse standing with other positions such as sitting or lying. Bridges are a great exercise for prolapse for many reasons, one being the posture that takes all gravity and downward motion off the pelvic organs and the pelvic floor.
Avoid unnecessary lifting and lugging and use aon organ supporting strategy when doing these tasks. The key is to not hold your breath and to have your pelvic floor working. Simply exhaling through a task like lifting can achieve this. We call this “blow before you go”.
Ensure a diet high in fruits and vegetables (lots of fibre) and a good toileting position to avoid straining.
When you feel the urge to have a bowel or bladder movement, head to the bathroom. Good toileting positions include having your knees higher than your hips – you can rest your feet on yoga blocks, on rolls of toilet paper, on the steps toddlers use for reaching the sink – as long as your knees are comfortably higher than your hips. Practice ‘opening’ and relaxing your pelvic floor: take a deep breath and go ‘GRRRRR!!’ Now take another deep breath and go ‘SSSHHH!!’ Which did you find the most ‘opening’ for your pelvic floor? Try making that noise the next time you have a bowel movement! It will help move things ‘down and out’ without stressing your pelvic floor. Now, put those steps together; sit on the toilet, knees higher than your hips. Lean forwards resting your elbows on your thighs. Make your noise (‘Grr’ or ‘Shh’ – whichever works best for you). When you are finished, do a pelvic floor contraction (close the opening around your anus and lift up and in) This signals to your brain that you are all done.
In some cases a pessary or vaginal supports can help undergird pelvic organs. They are used in conjunction with exercise and can be fitted for once off use or more permanently.
External support such as hideaway (a garment with elastic straps that allows for support over the perineum up to the pubic bone)
Internal assistance, such as Impressa (one time use bladder support), Uresta (silicone device for SUI) and silicone pessaries (silicone devices both for SUI and prolapse)
Pessaries are being used a lot more in younger women. I liken them to a sports bra for your vagina or a pair of reading glasses. They can be used only for bothersome activities such as running, skipping or doing a weight lifting class and then removed. This decreases the risk of adverse outcomes such as infection, abrasion and migration- (perforation of the vaginal wall and movement to other areas of the body).
So that concludes an overview of underactive pelvic floor structures.
Overactive Pelvic Floor
If we consider the overactive pelvic floor, the symptoms are usually not quite as apparent.
Vaginally, women will report a degree of resistance with inserting sanitary ware or with penetration. Both initial and deeper. Some state that they can shift or change position to ease the discomfort, while for others any form of penetration is uncomfortable.
A more holistic look at the sexual history experience and any trauma is obviously necessary but generalised heightened tension and stress levels can point to some upregulation the muscles.
This can be explained by the nerve supply to the pelvic floor structures. The majority is innervated by the pudendal nerve which is also under autonomic nervous system control.
So when we experience stress the pelvic floor muscle will usually tighten in response. Similar to clenching our jaw or bracing our shoulders.
The local up-regulation response is addressed with cognitive (top down), somatic (bottom up) as well as mindfulness strategies.
Bladder-wise, overactive bladder is another common presenting complaint.
Overactive bladder
Overactive bladder (OAB) is a condition where there is a frequent feeling of needing to urinate to a degree that it negatively affects a person’s life. The frequent need to urinate may occur during the day, at night, or both. If there is loss of bladder control then it is known as urge incontinence. More than 40% of people with overactive bladder have incontinence. Conversely, about 40% to 70% of urinary incontinence is due to overactive bladder. Overactive bladder is not life-threatening, but most people with the condition have problems for years.
The cause of overactive bladder is unknown.
Risk factors include obesity, caffeine, and constipation. Poorly controlled diabetes, poor functional mobility, and chronic pelvic pain may worsen the symptoms. People often have the symptoms for a long time before seeking treatment and the condition is sometimes identified by caregivers. Diagnosis is based on a person’s signs and symptoms and requires other problems such as urinary tract infections or neurological conditions to be excluded. The amount of urine passed during each urination is relatively small. Pain while urinating suggests that there is a problem other than overactive bladder.
Specific treatment is not always required. If treatment is desired pelvic floor exercises, bladder training, and other behavioral methods are initially recommended. Weight loss in those who are overweight, decreasing caffeine consumption, and drinking moderate fluids, can also have benefits. Medications, typically of the anti-muscarinic type, are only recommended if other measures are not effective. They are no more effective than behavioral methods; however, they are associated with side effects, particularly in older people. Some non-invasive electrical stimulation methods appear effective while they are in use. Injections of botulinum toxin into the bladder is another option. Urinary catheters or surgery are generally not recommended. A diary to track problems can help determine whether treatments are working. This bladder diary gathers information about type and quantity of fluid consumed, frequency of voiding and if and how much urine was lost.
Common bladder irritants include alcohol, caffeine, citrus, sweeteners and processed foods.
Overactive bladder is estimated to occur in 7-27% of men and 9-43% of women. It becomes more common with age. Some studies suggest that the condition is more common in women, especially when associated with loss of bladder control.
In layman’s terms overactive bladder can be irritated by ‘peeing just in case’. Voiding before leaving the house, when arriving at a destination or when asked to go to the washroom by your girlfriends at a party.
The normal feedback loops between brain, bladder and pelvic floor are changed and the bladder becomes relatively overactive.
When the pelvic floor is overactive it can itself irritate the bladder and contribute to overactivity.
The behavioural strategies that we address are the bladder irritants, as revealed in the bladder diary, and concepts around the fact that the bladder and pelvic floor are inversely proportional to each other.
When the bladder contracts the pelvic floor has to relax and conversely, when the pelvic floor contracts, the pelvic floor has to relax.
So when an urge is felt, contracting the pelvic floor will decrease the degree of sensation felt- either enough to defer the void or to allow time to get to the washroom without rushing and leaking.
If we further distract attention by asking for tricky mental tasks like counting backwards from 100 in 7’s, reciting telephone numbers, recipe ingredients or whatever takes concentration we can decrease the urge even more effectively.
If necessary, a timed voiding schedule can be instituted to get to 2-3 hours between voids.
Constipation
A very common concern for women is constipation. Gut transit times and gut motility can be slower in women, but the aim is still to pass at least one daily sausage-shaped bowel movement with ease.
Faeces is waste matter and need to be eliminated for optimal health. Especially hormones can be reabsorbed into the bloodstream affecting the balance the body is trying to achieve.
Pelvic floor overactivity can impact the required relaxation for an effective bowel movement, so addressing optimal toileting behaviour and positions is crucial.
When you feel the urge to have a bowel movement, head to the bathroom. Good toileting positions include having your knees higher than your hips – you can rest your feet on yoga blocks, on rolls of toilet paper, on the steps toddlers use for reaching the sink – as long as your knees are comfortably higher than your hips. Practice ‘opening’ and relaxing your pelvic floor: take a deep breath and go ‘GRRRRR!!’ Now take another deep breath and go ‘SSSHHH!!’ Which did you find the most ‘opening’ for your pelvic floor? Try making that noise the next time you have a bowel movement! It will help move things ‘down and out’ without stressing your pelvic floor. Now, put those steps together; sit on the toilet, knees higher than your hips. Lean forwards resting your elbows on your thighs. Make your noise (‘Grr’ or ‘Shh’ – whichever works best for you).
When you are finished, do a pelvic floor contraction (close the opening around your anus and lift up and in) This signals to your brain that you are all done.
Further to these common concerns I work with women on their fertility journey as well as in pregnancy.
Pelvic Girdle Pain
Pubic symphysis dysfunction or more correctly, pregnancy related pelvic girdle pain is the discomfort experienced along the pubic symphysis, groin or sacro-iliac joints.
Pelvic girdle pain is a protective output by the brain to get you to move a bit more mindfully and take things easier in general.
To decrease the perceived threat response, aim to move a bit more slowly and symmetrically (think getting into and out of a car, and turning over at night) and do some gentle pelvic tilting before you get up /change position.

Birthing
Another cornerstone of my approach is reviewing evidence based birthing strategies. This pertains to labouring and birth positions as well as breathing strategies to optimise pelvic floor outcomes.
(Can give more details if this comes up in discussion)
Postnatal care
This is perhaps the most popular time I connect with women.
I consider the kind of birth and birth experience the woman has had and evaluate the abdominal wall and pelvic floor.
DRA
There is a lot of talk about DRA, Diatsis Rectus Abdomins in the media.
In this condition the load transfer capacity of the midline connective tissue is impeded, causing the abdominal contents to bulge out and making the tummy look much bigger than it is.
Traditional abdominal activity can exacerbate the situation.
We need to approach the abdominal wall as part of a unit of muscles that control posture.
Your diaphragm, pelvic floor, lower abdominal wall and muscles supporting the spine.
Thus functional position and posture such as sleeping and breastfeeding are considered.
Further, the 4th trimester is a period of time in which the body is prioritising healing and its new homeostasis . Again, sleep, nutrition, support and stress resilience will all play crucial roles in optimising the outcomes.
Listen to the podcast HERE.

