I put this slideshow together to address some of the most common queries I hear about menopause and peri-menopause. It is intended to empower women to make informed choices and also give an opportunity to reframe the menopause experience.
Menopause has been heavily pathologized, a midlife ailment that need to be medicated and treated. Advertisements show women in distress over symptoms, while the words grumpy, fat and bitchy are synonymous with this life stage. And yet this concept of it being a disease is only really prevalent in the west, with the degree of bothersomeness correlating with higher socio-economic status. The more we adulate youth, the more disruptive the symptoms seem to be.
Eastern cultures, on the other hand, tend to venerate older women, making them leaders and matriarchs. Pillars of the society that are looked up to. Often these cultures and their languages do not even have words for hot flushes and night sweats.
Ladies, peri-menopause can be such a key opportunity to look at your overall health and well being. We get notifications from our body that things are in flux. It’s an opportunity to get our hormones checked out and re-asses food intake and poop output.
I want to move away from the notion that our body somehow fails us from the mid 40’s onwards. No, it’s talking and communicating with us and I want to encourage the art of listening to it.
We are a generations that will live half its life post-menopausally!!
Let’s do well so that we can empower the women and girls coming after us.
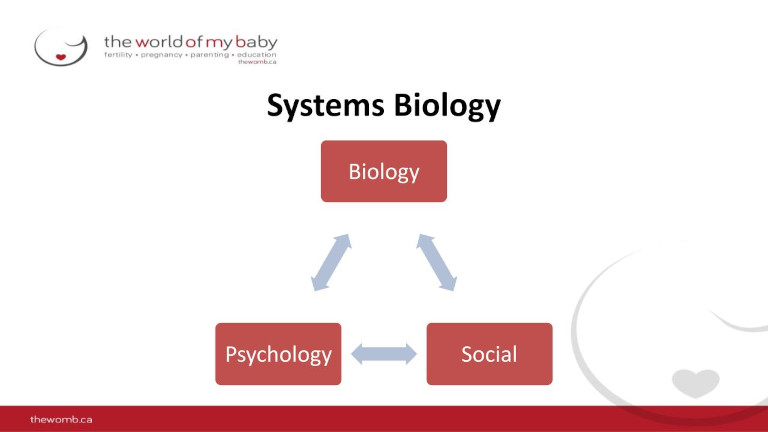
I will be discussing menopause through a bio-psych social lens, highlighting compounding factors that may negatively or positively impact this life transition.
Menopause is the term for the one year anniversary of the last period. It is a moment in time.
Before that moment you are in peri-menopuase, after that moment you are post-menopausal.
The mean age for menopause is 51 years of age.
Peri-menopause
- Can last 2-10 years , most women experience +- 3 years associated with hormonal imbalances
- Periods less regular, lighter bleeding
- hot flashes
A study presented at the 2019 conference of the North American Menopause Society found night sweats were linked to cognitive dysfunction in menopausal women, decreasing the ability to pay attention and perform higher-level thinking tasks.
Another found a direct link between the frequency and persistence of hot flashes and cardiovascular events later in a woman’s life. If you, or a friend, are really battling with hot flashes, a visit to your GP for a stress test may well be really beneficial.
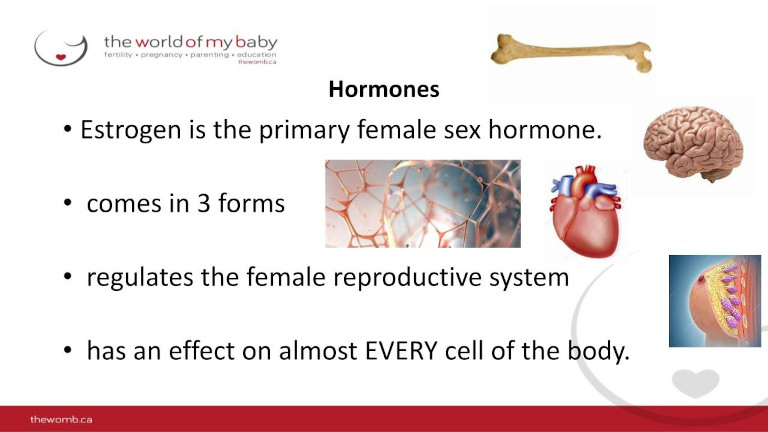
Estrogen comes in 3 forms. By far the strongest form is oestradiol which is secreted by your ovaries in your fertile years.
The form of estrogen secreted in the menopausal years called estrone. It is formed in the adrenal glands and fatty tissue (adipose tissue) and to a much lesser degree in the ovaries.
High estrone levels may increase the growth of breast cancer and uterine cancer especially in obese women.
Decreasing levels of estrogen impacts heart health, brain health, bone health negatively
In peri-menopause and menopause hormone ratios change:
The ratio of the 3 estrogen forms to each other changes as well as the ratio progesterone
Thyroid: T3, T4, TSH
Vitamin D3 levels
Cortisol
Cholesterol HDL and LDL
Fluctuations in any of these levels may lead to symptoms of lowered energy, weight gain, changes in hair growth etc.
A complete hormonal profiling done by ND may be advisable.
The adrenal fatigue theory suggests that prolonged exposure to stress could drain the adrenals leading to a low cortisol state. The adrenal depletion would cause brain fog, low energy, depressive mood, salt and sweet cravings, lightheadedness, and other vague symptoms.
Many women assume that the concerns they have at peri-menopause and beyond are to do with low estrogen. And while this is kind of true- estrogen and progesterone both decrease and they not decrease at the same rate leaving with you with are relatively higher level of estrogen. We call this relative estrogen dominance.
It is often experienced by women in their 40’s and a key feature is heavy , painful periods.
Other symptoms may include,
- irritability,
- weight gain,
- bloating and swelling
- tenderness in your breasts
- fibrocystic lumps in your breasts
- decreased sex drive
- irregular menstrual periods
- increased symptoms of premenstrual syndrome (PMS)
- mood swings.
- headaches.
These features mimic peri-menopausal symptoms and are often brushed off as such.
If these symptoms are familiar to you, it may be a good idea to consult with a naturopathic doctor.
Most meat we buy is filled with hormones and antibiotics and can drive this estrogen dominance. Plant-based protein is a great way to meet protein requirements, increase fiber intake and keep gut bacteria happy to ensure good stool formation.
Xeno oestrogens are similar to estrogen but have a negative effect on the body. They are found in plastics, herbicides, household cleaners, personal care products and cosmetics and the birth control pill.

Hormones aside, the fifth decade can have some psychosocial triggers that can cause stress of its own.
This stress can exacerbate menopausal symptoms.
Children are often moving out of the house, some people retire or are caring for ailing parents. Change is difficult and can often trigger low mood and and/or feelings of anxiety.
It is also important to honour that menopause itself bring about feelings of grief: loss around childbearing, body changes, sexuality, and aging.
All of these impact the HPA(hypothalamic pituitary adrenal) axis- our stress system axis.
This axis intertwines your hormones with your nervous system and attempts to regulate out mood and energy levels.
This is a key area to investigate further if you’re feeling overwhelmed and stressed.
Urogynecological Considerations: The Pelvic Floor and More.
In Menopause the uterus, cervix and ovaries decrease in size. Notably the clitoris also becomes smaller and may contribute to the decreased arousal women report. Stimulation of the clitoris may not lead to the same degree of arousal that it did previously.
(on a side note, the clitoris has about 8000 nerve endings, double as much as the penis)
The fat in the labia majora and the mons pubis decreases and pubic hair becomes sparse.
Cervical mucus decreases until they disappear completely
The genitourinary syndrome of menopause (GSM) is a new term that describes various menopausal symptoms and signs including not only genital symptoms (dryness, burning, and irritation), and sexual symptoms (lack of lubrication, discomfort or pain, and impaired function, but also urinary symptoms (urgency, dysuria, and recurrent urinary tract infections).
45 to 63 % of menopausal women report symptoms.
These symptoms are all directly linked to decreased estrogen levels and these changes reduce elasticity of the vagina, increase vaginal pH, lead to changes in vaginal flora, diminish lubrication, and increase vulnerability to physical irritation and trauma.
Factors that can contribute to excess oestrogen in the body are poor clearance via the liver and colon. Gut health and good bowel function are key factors to look at.
How often are you having BM and how well is your liver functioning? Remember, alcohol and medication all need to be broken down in the liver so it may not be effectively clearing excess estrogen.
To minimize this impact and transition through menopause more easily we need to look at the four pillars of health.
Get tested!!!
So what now:
Seek professional advice and or discuss your most bothersome symptoms
Is it depression?
Is it anxiety? Is it anger, rage, fatigue, brain fog.
Start with one small manageable change that looks like self care. Not another to do list item.
Movement:
It is probably the most important aspect as it modifies all the other pillars
It is beneficial for stress management which in turn helps us make better food choices (as we do not waste the effort we put into exercising)
It lowers circulating cortisol levels which has been shown to contribute to fat deposition along the waist
It can help moderate hot flashes as it has a beneficial effect on the thermoregulators in our body.
It builds/maintains muscle mass.
It slows down the loss of bone density.
It improves our cardio vascular function. 1 in 2 women will experience a cardiovascular event in their lives and it is the biggest killer of women.
It is good for mental health.
Restorative: Breathing, walking, yin yoga.
Strength training: Bone, joint, tendon health- glut med and max development
Nutrition:
The foods that we eat can either nurture or harm our gut bacteria.
Highly processed and refined, sugary foods drive inflammation in our system and exacerbate the symptoms of altered oestrogen levels and contribute to auto-immune diseases and cancer.
Our body eliminates excess oestrogen via the gut- well formed, daily poops are essential.
Choose a diet based on the Mediterranean one to optimize nutrition and help form good stool.
- Minimally processed vegetables, fruits and whole grains in season.
- Oily fish, eggs and nuts and seeds as protein sources.
- Lots of water.
Stress management:
- Where are your stress levels at?
- What strategies work and which ones can you incorporate on a daily basis.
- Walking, chatting with a friend, sipping a favourite drink, playing with a dog, stroking a cat…. Doing something that sparks JOY.
Sleep:
- What is your sleep like? Interrupted?
- By what, when?
- Sleep hygiene: no screens 2 hours before bed, no phones near your bed, dark room, breathable fabrics.

