Notes for prolapse and pessary webinar 21 April 2022
Good evening ladies!!
Thank you so much for joining me on this webinar or catching the replay!
My name is Gerda Hayden and I am a pelvic health PT working out the WOMB (the WORLD of my baby) in Burlington, Ontario. It’s a perinatal care clinic with a holistic multi-disciplinary approach.
I have a special interest in prolapse and prolapse care through the entire life span, so was really excited when the team at Corelife asked me to give a talk on the subject.
You will find my contact details at the end of this presentation so please do not hesitate to reach out!
We will look at the prolapse presentation, some contributing or risk factors and then talk about management, including pessary use.
I want to emphasise that these are principles and not a one size fits all approach. A million Kegels are not the answer to addressing prolapse!!
Before explaining what prolapse is, I’m going to take a moment to reframe our understanding of anatomy as it shapes our prolapse experience.
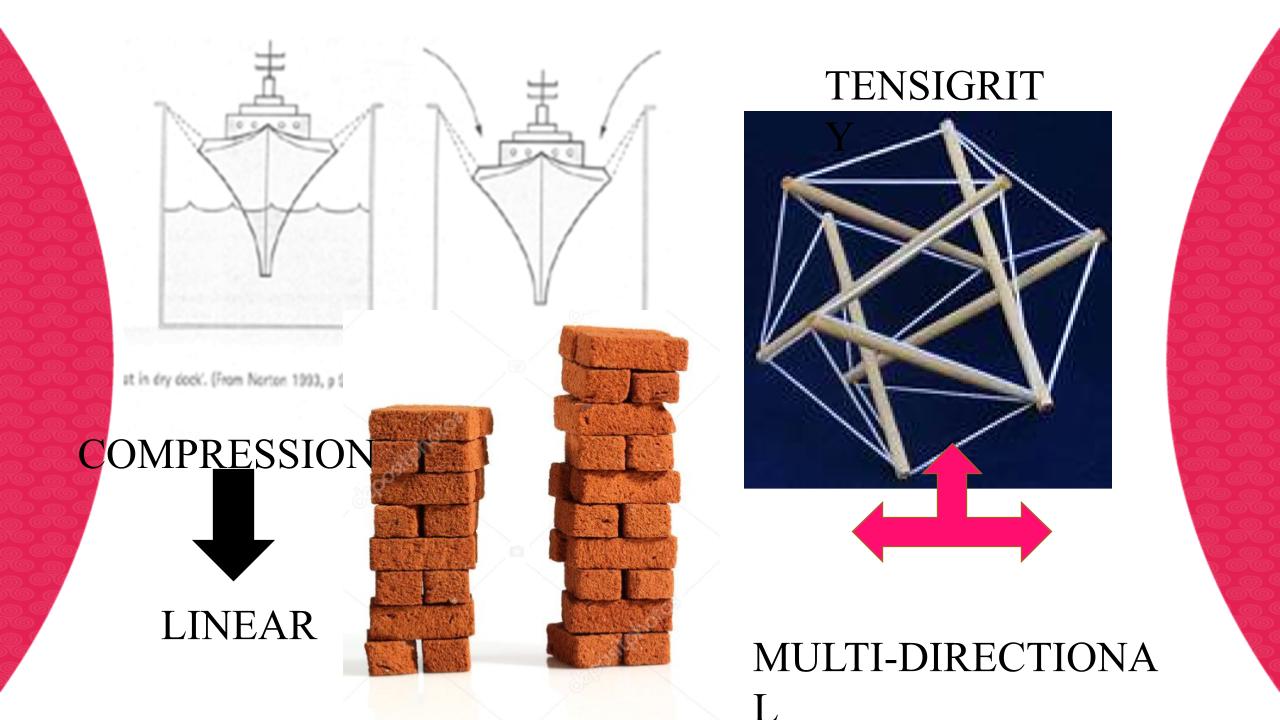
For a long time we considered the bones to be a stack of rigid blocks stacked on top of each other.
And the muscles and tendons and organs were essentially draped in between and over the bones. We moved as result of forces, pulleys and levers acting on the bones .With that model in mind any pelvic organ movement is considered a collapse, or a linear downward movement, a falling down of the tissue.
Our understanding of anatomy has fundamentally changed though and we are now realising that instead we demonstrate a model more like this image here. It’s called a tensegrity model, where the muscles and fascia, the elastic components are constantly pulling, while the bones, the rigid components, are pushing. And if all the parts are optimally organized we have this dynamic balance, where the rigid structures don’t touch and everything has lots of wriggle room. So we can move freely in all kinds od different directions and positions and the forces are transmitted in many ways all of the time. We can move freely, do complicated yoga positions, stand on our head and have babies.
We are self-suspended within our elastic components, most notably the fascia which connects everything to everything.
It’s these elastic elements that allow minute alterations and responses to internal pressures and the external world we move in.
Now, when these tissue elements have sustained and injury, the tissue tends to be a bit stiffer and cause some restrictions in movement. In the pelvis these restrictions can occur after tissue injury with birth. This can mean that the soft squishy organs, the bladder, the uterus and the rectum are not optimally aligned and they are the pulled against the vaginal wall which we then experience as a prolapse.
So to recap, it’s not a downward falling, it’s a pulling of tissue that occurs.
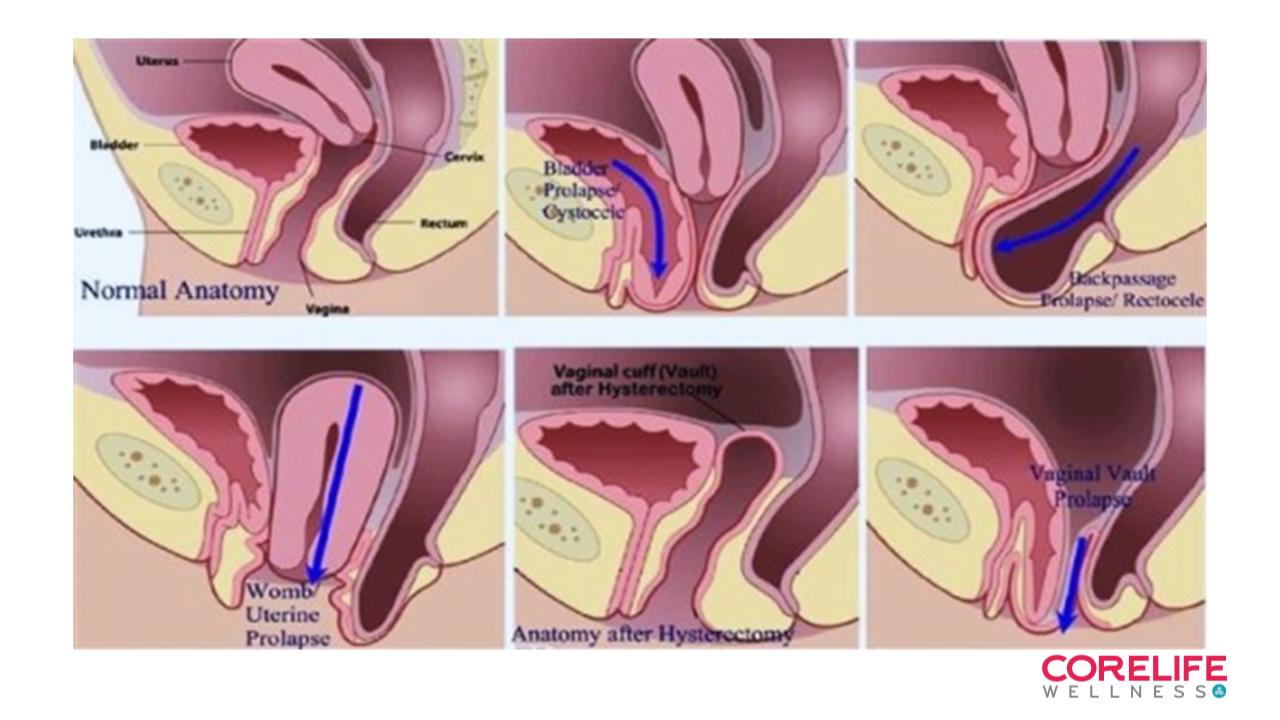
Now that we have addressed the mechanism of prolapse, let’s chat about the different types of tissue changes you may present with.
The top left shows the ideal position of the organs suspended within their connective tissue web. (Except that the connective tissue isn’t shown)
Top middle shows movement of the bladder or cystocele. In practice I find the bladder is often deviated to the Left after a vaginal birth.
Top right shows a rectocele. In practice I find these occur with perineal body restrictions.
Bottom left shows a hysterocele, womb movement, and the findings in practice are more of a cervic pulled to the right or left.
The bottom pictures on the right depict anatomy after a hysterectomy and what can happen if the vaginal vault deviates.
So, lets look at the risk factors
We have some acute ones, mainly to do with birth and some as result of sustained or repeated forces onto the pelvic floor.
In response to these occurrences, we get some connective tissue changes, generally tissue becomes stiffer- less flexible and less able to optimally suspend itself. And thus suspend the pelvic organs/
The tissue is impaired , not just always ‘weak’
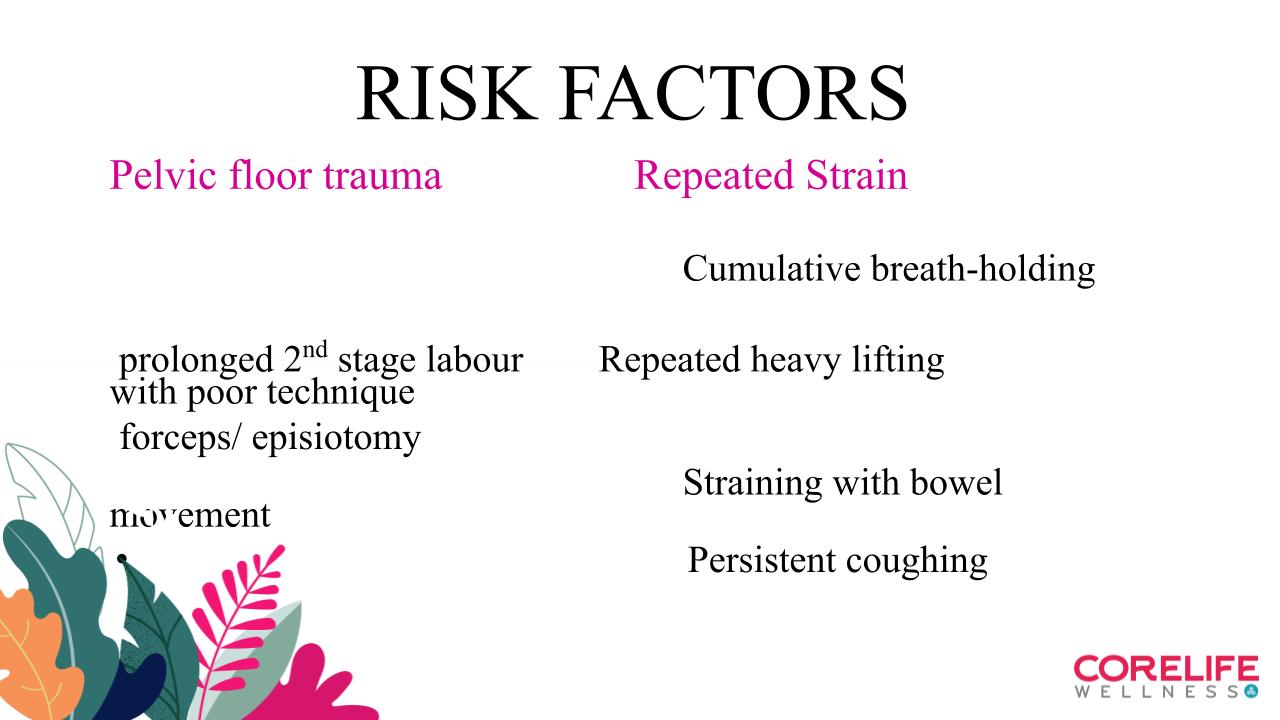
So, lets look at the risk factors
We have some acute ones, mainly to do with birth and some as result of sustained or repeated forces onto the pelvic floor.
In response to these occurrences, we get some connective tissue changes, generally tissue becomes stiffer- less flexible and less able to optimally suspend itself. And thus suspend the pelvic organs/
The tissue is impaired , not just always ‘weak’
So what are the symptoms of prolapse.
Women report a sense of dragging, heaviness, bulging, difficulty initiating urination
Or a sense that , and I’m parapharsing’ something isn’t ‘quite right down there’
The most cited prevalence is fairly high at 50%, but only 15% are SYMPTOMATIC after 20 yrs.
The threshold at which prolapses ae diagnosed is not clearly defined in the literature.
Prevalence rates are actually fairly inconclusive, as it depends on the practitioner’s threshold of reference. Your midwife, family Dr, OBGYN etc May or MAY not give you a diagnosis, based on what their perception of prolapse is.
We are recognizing that the vaginal tissue is very elastic and that some degree of organ movement is to be expected after birth and also with significant changes to intra=abdominal pressure.
Grading or staging of prolapse is also being debated, so I tend to work with a women’s perceived degree of bother. Using a questionnaire.
Management: how do we saftely get active with POP
- Modifying risk factors: pregnancy PT care, informed birth choices
- Addressing tissue changes: scar tissue, adhesions, organ deviations THROUGHOUT The body.
I assess breath strategies, standing posture as well as sit to stand and walking to determine and address any restrictions
- supervised pelvic floor muscle training: this can be either strengthening or Lengthening depending on the findings. The 2019 return to running guide gives a framework for understanding what the strength, endurance, co-ordination and lengthening capacity of the pelvic floor should be for optimal tissue support. Our pelvic floor act like trampolines cushioning impact and should feel like that too on palpation.
- We are optimizing postural pre-activation control as well as larger mover muscles strength and endurance
- guidance related to
-Intrabdominal Pressure management
-General movement
-Diet
- Pessaries
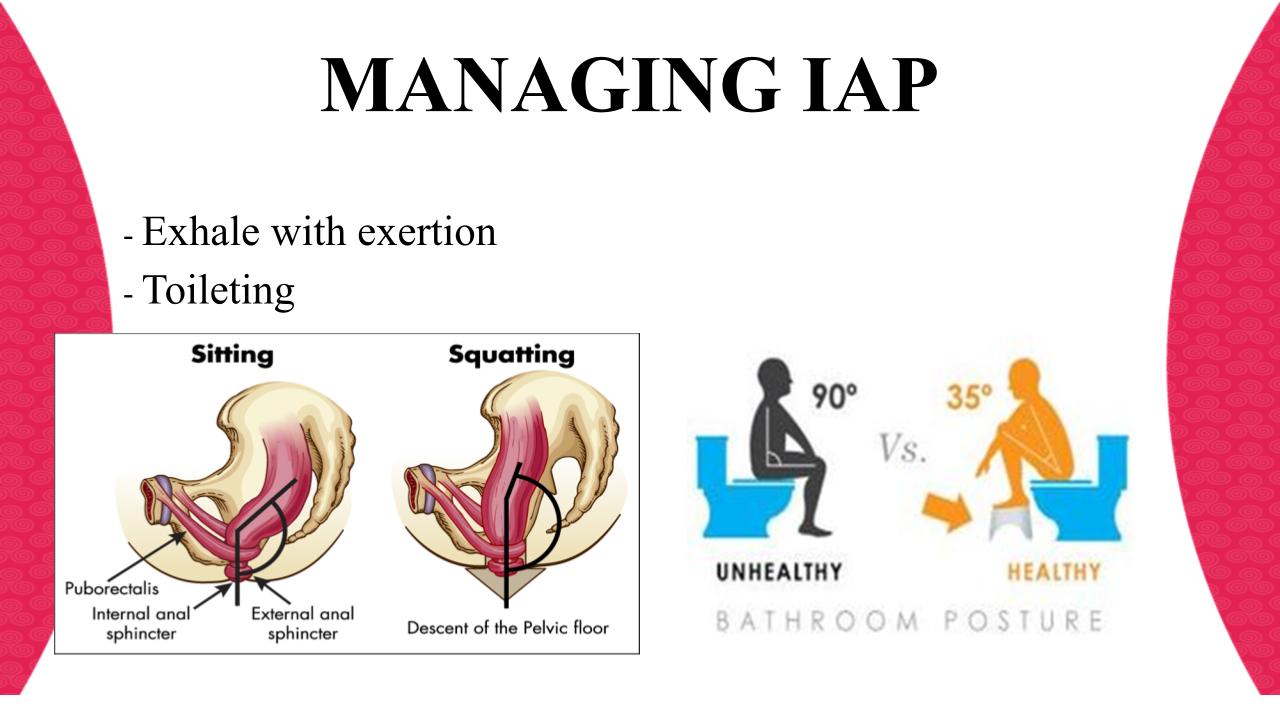
So, regardless of when your prolapse has presented, be it post partum, or peri-menopausally or anywhere in between, I’ll start with IAP management.
IAP is the term given to the increase in pressure in your abdomen in response to movement. The connective tissue elements respond to these pressure changes.
One of the activities that increases IAP the most has actually been found to be sit to stand! And we all do that OFTEN throughout the day.
Managing IAP well can have huge benefits for optimizing pelvic floor function. ( I won’t get into all the anatomical details here..), suffice to say
I highlight breath strategies with moving and lifting as well as good toileting positions.
When it come sto considering actual vaginal tissue integrity, I consider the elasticity and resilience of the organ.
If tissue appears thin or sensitive, I also consider either a hyaluronic acid cream or some vaginal estrogen to optimise collagen health.
Finally, I also need to consider what else is going on in a 24 hr period.
What nutrients are being consumed- are they predominantly inflammatory or anti-inflammatory as that influences our overall well-being and are also the building blocks the body uses to repair themselves
Sleep: how much are you getting and what is it’s quality
Movement: what were you doing, what are you doing currently, what do you want to get to?
We brainstorm types, amount and what exercise resonates with you. I have very few taboo exercises, rather I’d modify what you enjoy doing. Cause if you don’t enjoy it, you’re not going to do it!!
Stress: what is your perception of the degree of stress you are under and what startgies do you choose to deal with your stress? For so many women running is more a mental headspace thing than just an exercise.
And sometimes we get about 80%there and some movements remain uncomfortable.
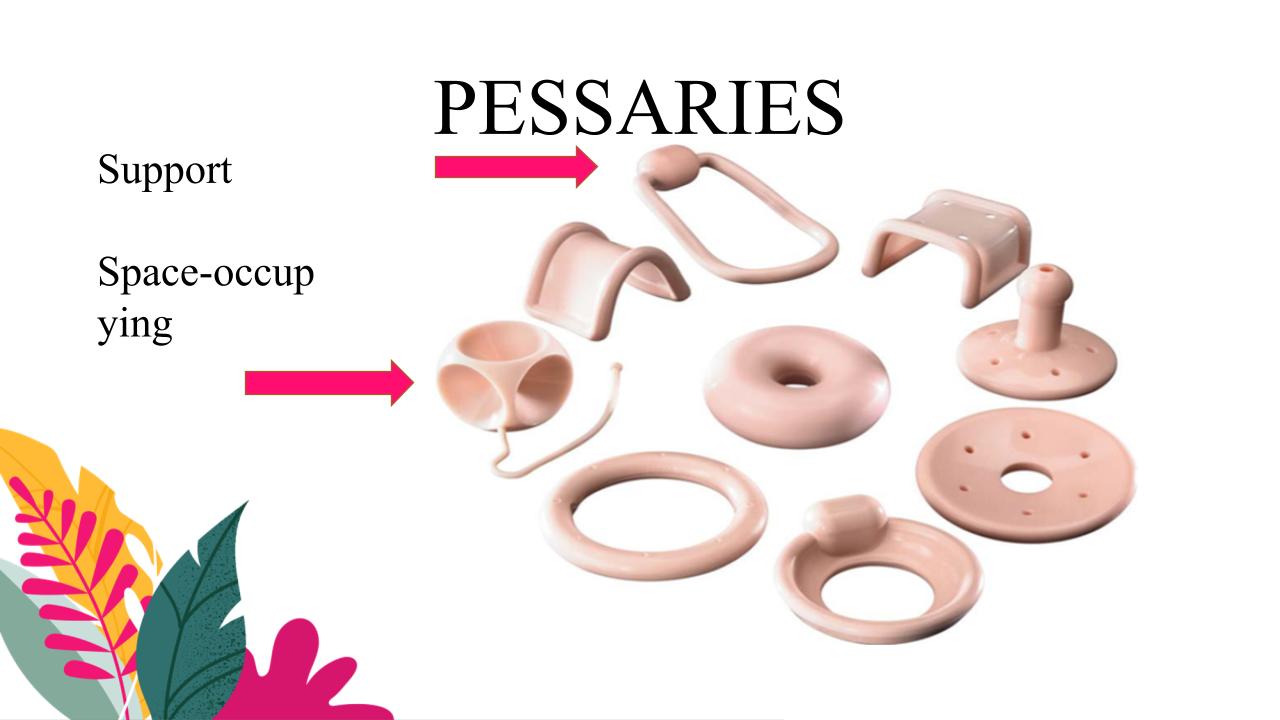
And then we can talk pessaries!!
A pessary is a prosthetic device that can be inserted into the vagina to support its internal structure
There are two main types of pessary: support and space-filling. They come in many different shapes and sizes to fit a woman’s individual anatomy. They are all usually made from medical-grade silicone, which makes them durable and resistant to absorption.
The most commonly used support pessary is the ring pessary with support. This is because it fits a large majority of women and can be used at all stages of pelvic organ prolapse.
The most commonly used space-filling pessary is the Gellhorn pessary. This has a broad base with a stem that comes in different lengths so that it will also be able to fit most women.
Fitting is a trail and error exercise with the aim of finding a pessray that supports but is not felt once inserted.
Squatting, walking, sit to standing and toileting are all trialed and once the correct device has been found, a medical professional needs to sign off on any contra-indications, before the device is ordered.
Possible complications
Vaginal or urinary infection:
▪ If there are signs or symptoms of infection, you must remove your pessary and consult your doctor.
▪ Candida, bacterial infection or urinary tract infection are the most commonly seen and require a diagnosis and the appropriate treatment.
Bleeding:
Erosion, ulcers, laceration and inflammation of the vaginal mucosa are more common if the pessary fits too tightly or if the mucosa is atrophied or not healthy. Bleeding may also occur if the pessary was forgotten inside the vagina.
It will require you not no wear the pessary during medical treatment
Incarceration: when the pessary is stuck in the mucosa and cannot be removed
(Do not try to remove it, it will bleed!! ) You will be referred to your doctor or gynecologist)
Migration: when the pessary moves from the vagina to the bladder or
the rectum and creates fistulas
these risks are mitigated however by suggesting frequent removal of the pessary to allow the vaginal wall time to repair itself.
I re-evaluate the pessary annually to determine fit, comfort and possible wear and tear of the silicone.
And there we have it ladies.
Caring for the device
If you are comfortable removing and reinserting your own pessary, you may remove the pessary once or twice a week. Once removed, clean it with mild soap and warm water and then rinse before replacing it. You doctor may prescribe a vaginal estrogen cream to apply inside your vagina while the pessary is out to prevent irritation.
Pessaries can fall out if you strain. If you can, try not to bear down during bowel movements. If the pessary does fall out, you can reinsert it after you clean it.
Many women find insertion easier when they are standing up with one foot resting on a stool. It’s important to use plenty of water-based lubricant for insertion.
If you aren’t comfortable removing and reinserting your own pessary, your doctor will set up follow-up visits for you to come and it done in the office. Frequency of visits can range from monthly to every three months, depending on your needs.
When to see a doctor
A pessary can occasionally cause some complications:
- Foul-smelling discharge. This could be a sign of a condition called bacterial vaginosis, which is an imbalance in the natural bacteria found in your vagina.
- Irritation and even damage inside the vagina.
- Bleeding.
- Passing a small amount of urine during exercise or when you sneeze and cough. This is called stress incontinence.
- Difficulty having sexual intercourse.
- Urinary tract infections. Initial signs of this may be difficulty urinating, feeling unwell, or a high temperature.
It’s important that you see your doctor if you develop any signs of these complications, as they are usually very treatable.

